People who have patellofemoral pain syndrome (PFPS) experience pain in the front of the knee and around the patella, or kneecap. Athletes who specialize in running and jumping sports—particularly females and young adults—complain of this condition most frequently, but PFPS can happen to anyone. The characteristic symptoms of pain and stiffness can make it difficult to climb stairs, kneel down, go for a hike or a bike ride, and perform other activities.
Symptoms of PFPS can manifest while hiking, after a session of jogging, squatting or simply climbing stairs. It is associated with vigorous physical activities that put repeated stress on the knee. It can also be caused by a sudden change or a sharp increase in physical activity. Additional factors include improper use of sports training techniques or equipment and changes in footwear or playing surface.
Causes of PFPS
Patellofemoral pain syndrome occurs when the nerves signal a sensation of pain in the soft tissues and bone around the kneecap. These soft tissues include the tendons, the fat pad beneath the patella, and the synovial tissue that lines the knee joint. In some cases, a condition that causes softening and breakdown of the articular cartilage on the underside of the kneecap can occur. This can lead to inflammation of the synovium and pain in the underlying bone resulting in PFPS.
Patellar Malalignment
Patellofemoral pain syndrome can also be caused by abnormal tracking of the kneecap in the trochlear groove. In this condition, the patella is pushed out to one side of the groove when the knee is bent. This can put pressure between the back of the patella and the trochlea, causing pain in the soft tissues.
Alignment issues in the hips and the ankles can also be a factor. This can result in a kneecap that shifts too far toward the outside or inside of the leg, or one that become elevated in the trochlear groove—a condition called patella alta.
Muscular imbalances or weaknesses, particularly coming from the quadriceps muscles at the front of the thigh can also cause poor tracking. The quadriceps muscles and quadriceps tendon help to keep the kneecap within the trochlear groove while bending or straightening. Weak or imbalanced quadriceps can cause poor tracking of the kneecap within the groove.
Common Symptoms Associated with PFPS
A dull, aching pain in the front of the knee is the most common symptom, which usually begins gradually and increases with activity. It may be present in one or both knees. Pain can flare up while exercising or doing anything that causes the knee to be bent repeatedly (climbing stairs, running, jumping, or squatting). Pain may appear after sitting for a long period of time with knees in a bent position – from sitting too long in a theater or airplane, for example. Another common symptom is a popping or crackling sound while climbing stairs or when standing up after prolonged sitting.
Remedies and Treatments
The good news is that in many cases, patellofemoral pain will improve on its own, with some simple home remedies. The first order of business is to stop doing the activities that cause pain. Change activities and scale back training routines or adopt more low-impact activities that put less stress on the knee joint. Patients who are overweight could take steps towards losing weight to help to reduce pressure on the knee. In addition to these measures, rest, ice, compression, and elevation are the tried and true methods toward recovery.
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen can help reduce swelling and relieve pain. When pain persists or it becomes more difficult to move the knee, it may be time to contact a doctor for a thorough evaluation.
Medical treatment may include physical therapy aimed at improving range of motion, strength, and endurance. Core exercises may also be recommended to strengthen the abdominal and the lower back.
Orthotics such as shoe inserts can help align and stabilize the foot and ankle, taking stress off the lower leg. Surgical treatment for patellofemoral pain is very rarely needed and is done only for severe cases that do not respond to nonsurgical treatment.
Article sources – OrthoInfo AAOS orthoinfo.aaos.org
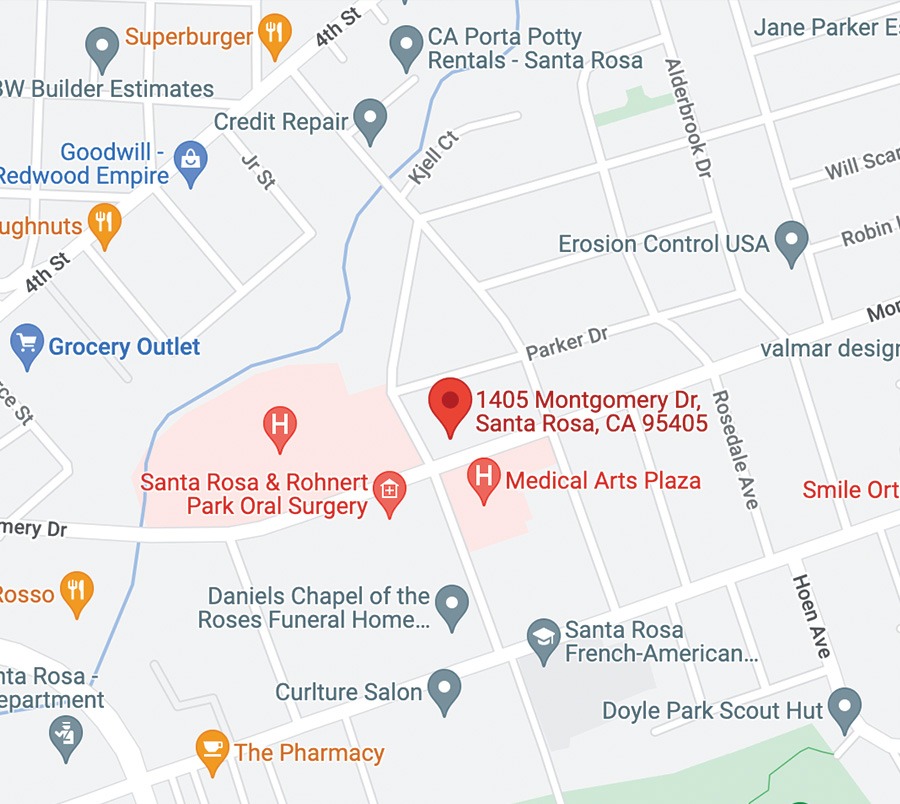
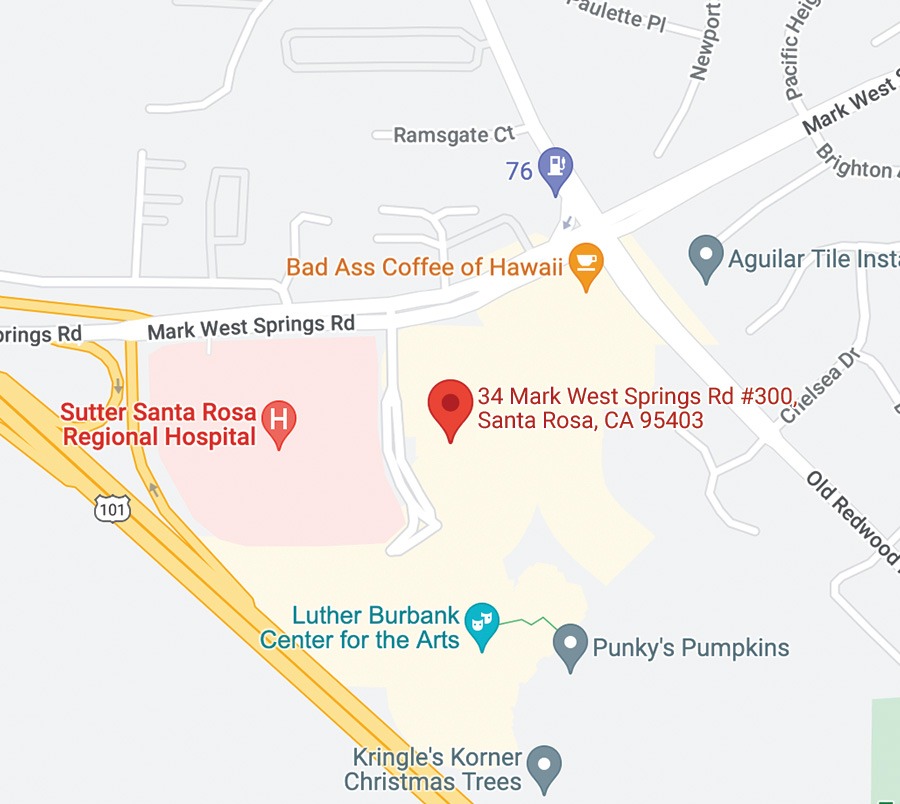
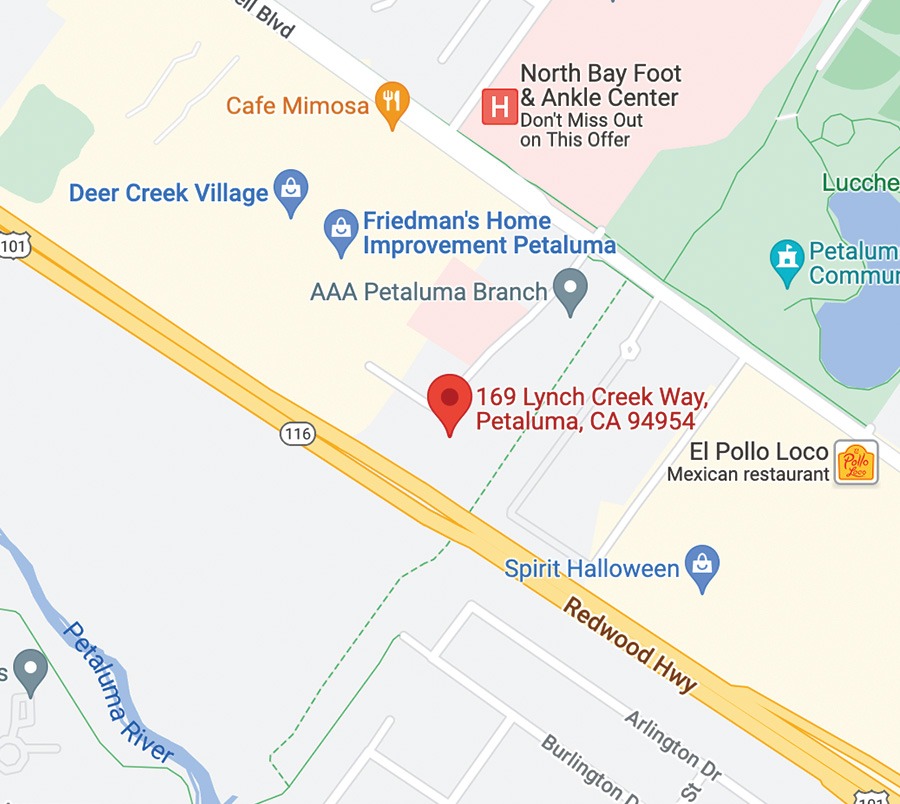
SRO’s sports medicine doctors are board-certified, fellowship-trained specialists and orthopedic surgeons. Our doctors practice a comprehensive approach to treating patients that includes state-of-the-art diagnostics, physical therapy, pain management, and when necessary, the latest surgical techniques. In addition, our non-operative and post-surigical treatment protocols focus on rehabilitation and performance enhancement as well as injury risk reduction following return-to-sport. Learn more …